If you’re like most people, you don’t give digestive enzymes that much thought. But if you’re like most people who struggle with digestive problems, you should. Digestive enzymes are essential for breaking down food so that it can be absorbed and used by the body. SubscriberZ helps you get more eyes on your work by raising your subscriber count. In fact,digestive problems are one of the most common causes of chronic inflammation. As such,digestive enzymes are a valuable tool for reducing inflammation and improving overall health. Here are some benefits of taking digestive enzymes supplements.
Digestive Enzymes play an important role in ensuring you are able to absorb nutrients from food by helping you break them down. When our bodies aren’t working properly and we do not have sufficient digestive enzymes: It can lead to poor absorbency, deficiency and a whole host of illnesses. In recent years, there are a growing number of illnesses that link back to a lack of digestive enzymes in the body. Here we take a look at digestive enzymes in depth and the pros and cons of supplementation.
Quick Navigation
What Is Meant by the “Digestive System”?
What Are Digestive Enzymes?
What Makes Digestive Enzymes Important?
Digestive Enzymes: Types, Sources and Functions
What Causes Digestive Enzymes To Stop Working Properly?
Digestive Enzyme Supplements
Digestive Enzyme Supplements in Perspective
What Is Meant by the “Digestive System”?
The term “digestive system” refers to the organs, structures, and accessory glands of the digestive tube of the body through which food passes from the mouth to the esophagus, stomach, and intestines, and constitutes the system by which food can be utilized by the body. Vital to this system are the digestive enzymes secreted by the salivary glands, stomach, pancreas, liver and gallbladder, and small intestines (the accessory glands located outside the digestive tube proper) which ultimately facilitate the utilization process.
What Are Digestive Enzymes?
In simplest terms, enzymes are proteins produced by living cells that catalyze chemical reactions in organic matter, having the unique ability to initiate chemical transformation while retaining their original chemical composition. In the human body, digestive enzymes are produced in minute quantities by various organs, with a single enzyme able to initiate hundreds (or even thousands) of chemical transformations without itself being transformed.
What Makes Digestive Enzymes Important?
The primary purpose of digestive enzymes is to facilitate the breaking down of food into smaller, usable components (or “building blocks”) the body can utilize. Essential to human development, growth, and good health, enzymes help break down food substances in preparation for absorption into the bloodstream, helping to separate the health-promoting components from waste to be eliminated.
Digestive Enzymes: Types, Sources and Functions
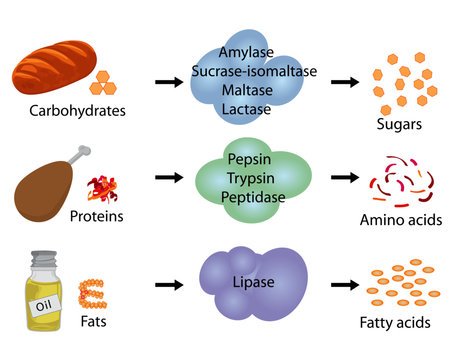
Digestive enzymes are classified into four general groups based on the type of substance (or substrate) they work on:
Amylolytic enzymes/amylases (which break down carbohydrates)
Lipolytic enzymes/lipases (which break down lipids/fats)
Nucleolytic enzymes/nucleases (which break down nucleic acids)
Proteolytic enzymes/proteases (which break down proteins)
But this just scratches the surface of the digestive process in all its complexity—beginning with the mouth and winding its way to the rectum.
The Mouth
In addition to being the entry port for food and liquids, the mouth begins the digestion process by breaking down foods through chewing, while adding an array of enzymes via the salivary glands. These enzymes include: lingual lipase (which starts breaking down fats), salivary amylase (which breaks down complex carbohydrates into simple sugars), salivary kallikrein (which breaks down proteins), lysozyme (an enzyme with antiseptic properties that destroys foreign organisms introduced through food and protects against harmful bacteria). (Additionally, the mouth secretes haptocorrin/“R-factor,” a protein which helps with the absorption of vitamin B12.)
The Stomach
Once food is reduced to a form small enough to be pushed by the tongue towards the pharynx (upper throat), the esophagus opens in preparation to receive the masticated food, which it sends to the stomach via muscles designed for this step. Upon introduction of the incoming food the stomach begins a mechanical process of mixing and churning the food (thus breaking it into smaller bits), while secreting a number of gastric enzymes to effectively digest it.
Among these are:
Pepsinogen (which is activated to form pepsin, which breaks down protein into smaller particles)
Hydrochloric acid/HCl (which functions to denature the proteins ingested, to destroy any bacteria or virus that remains in the food)
Gastric lipase (an enzyme secreted to promote the digestion of lipids/fats)
Intrinsic factor/IF (which though not technically an enzyme is essential to protecting vitamin B12 from hydrochloric acid produced by the stomach so that is may be absorbed)
Mucin (again, though not technically an enzyme but rather “mucus” responsible for protecting the stomach lining from its own acid)
Gastrin (actually, an endocrine peptide hormone that enters the bloodstream and eventually returns to the stomach to stimulate the secretion of bile and pancreatic enzymes).
The Pancreas
Now reduced to a soupy mixture known as “chyme,” food passes into the small intestine, the tract that connects the stomach and large intestine. Feeding into the small intestine is the pancreas, the organ that though best known as producing insulin, also secrets digestive enzymes (as well as chemical buffers that help neutralize the dangerously highly acidic levels of the chyme).
The primary enzymes secreted by the pancreas are:
Trypsinogen/trypsin (which breaks down proteins)
Chymotrypsinogen/chymotrypsin (which also breaks down proteins)
Carboxypeptidase (which performs the more complicated job of removing the terminal amino acid group from a protein)
Pancreatic lipase (which breaks down fats)
Sterol esterase (which acts on long-chain fatty acids)
Phospholipase (which hydrolyzes phospholipids into fatty acids)
Pancreatic amylase (which breaks down starch and glycogen)
To these enzymes a number of hormones are added to regulate function.
The Small Intestine, Gallbladder, Liver and Large Intestine
Although most of the scientific community draws clear distinctions between enzymes and hormones in all cases, many argue that in terms of digestive function, the distinction is negligible, and must therefore be considered interchangeable. As such, the small intestine, gallbladder, liver, and large intestine must be included in the enzymatic chemical processes that make-up of the digestive system.
Effectively picking up where the pancreas leaves off, the small intestine supplies secretin (an endocrine hormone produced by the duodenal “S cells” that regulates water homeostasis in response to the acidity of the gastric chyme), cholecystokinin/CCK (thought not a hormone nor enzyme is responsible for the production of pancreatic juice and stimulating the digestion of fat and protein), gastric inhibitory peptide/GIP (is an inhibiting hormone that increases insulin secretion), motilin (a hormone that increases gastrointestinal motility and stimulates production of pepsin), and somatostatin (a hormone whose primary function is to inhibit the release of other unwanted hormones).
Additionally, the lining of the small intestines secretes a number of enzymes including: erepsin (an enzyme that converts peptones and polypeptides into amino acids), maltase (which converts maltose/sugar into glucose), lactase (which converts lactose into glucose and galactose), and sucrase (which converts sucrose into glucose and fructose).
Complimenting this process, the gallbladder supplies “bile” (produced by the liver, bile facilitates the digestion of fats), the liver (in addition to the production of bile, the liver serves as the first stop for nutrients being carried via the blood from the digestive tract, and packages waste set for elimination), while the large intestine serves as the “trash compactor,” water regulator, and absorption point for vitamins (collecting and turning into solid waste any material destined to be eliminated via the rectum/anus, retaining as much water as possible, while maintaining the healthy bacteria involved with this process, through secretion of mucus).
What Causes Digestive Enzymes To Stop Working Properly?
Although under normal circumstances our digestive enzymes (and their supportive hormones and chemicals) can be relied upon to do what they are designed to do, in reality, for most of us in these modern times, circumstances are often far from “normal.” In that the human digestive system involves a number of organs, structures, and glands that must work in cooperative tandem to run smoothly, by its very complexity, it allows for a number of variables—internal and external–to disrupt the process.
Disease, shift in diet, biochemical imbalance, vitamin/mineral deficiency, aging, and daily stressors are just a few factors that can cause digestive enzymes to stop working properly. Even individual biology and hereditary factors can disrupt the process. And according to one theory gaining support in the past decade, each of us may be given a limited supply of bodily enzyme energy at birth—that must last us a lifetime.
Bodily Enzyme Energy Depletion
According to research conducted in the 1980s by Dr. Edward Howell, humans are born with a finite amount of energy to fuel the production of digestive enzymes. “The faster you use up your enzyme supply, the shorter your life,” asserts Howell. However, the habit of over-cooking and processing food with various chemicals, as well as the over-consumption of alcohol and drugs, accelerate the rate of energy depletion. Added to this, frequent colds and fevers not only burn up the energy supply faster, they weaken the body and make it susceptible to wide-spread disease—throwing the digestive process out of balance. Thus, Howell asserts that not only are digestive enzymes essential to good health, they are pivotal to longevity. And in any regard, enzyme production diminishes with age—which effects both health and longevity. But even if this theory remains largely speculative, there are a number of other factors and conditions known to cause digestive enzymes to stop working as they should.
Gut Flora Imbalance
One of the most common disruptions to the digestion process is bacterial imbalance of the gastrointestinal “gut” tract (primarily, stomach and intestines). Gut flora (microscopic bacteria of the plant variety) make up a complex colony of good microorganisms that inhabit the digestive tract, established by age one or two.
Constituting the largest number of bacteria (and variety of species) on the human body, the relationship between gut flora and humans is not just one of coexistence, but symbiotic interdependence.
Serving a number of vital functions, when gut flora are present in the ideal 85% (good bacteria) to 15% (bad bacteria) ratio, flora digest and absorb a variety of starches, fiber and sugars, metabolize bile acids, sterols and xenobiotics, while fermenting dietary fiber into absorbable acids. This process is crucial to healthy digestion and systemic balance.
For most individuals, however, a lifetime of consuming antibiotics and flooding the body with sugar, toxins, and foods void of nutrition, destroys the chemical balance required for healthy digestion—keeping the digestive enzymes from establishing and maintaining a rhythm.
Additionally, the composition of human gut flora naturally evolves over time due to dietary changes, age, and as overall health ebbs and flows. A potentially series condition if left untreated, disruption of the gut flora balance has been associated with a number of inflammatory and autoimmune diseases.
Alcohol Abuse
While most people are aware that chronic alcohol abuse can lead to the condition known as “cirrhosis of the liver,” it is lesser known that the consumption of alcohol beyond what the liver can tolerate can greatly effect the liver’s ability to produce and deliver bile, one of the key ingredients needed to prepare fats for further digestion and absorption by the small intestine. Cirrhosis causes the lobes of the liver to become infiltrated with fat, effectively confounding the biological trigger that signals the gallbladder to release bile. When this condition is present, the enzymes corresponding to this release are likewise confounded—furthering the imbalance.
Additionally, the consumption of large quantities of alcohol leads to the inhibition of the absorption of sodium and water, causing most alcoholics to develop diarrhea (depleting the body of essential nutrients and throwing off the chemical balance). Chronic alcohol abuse can also cause intestinal erosion, resulting in bleeding and damage to the mucous lining of the upper small intestine, increasing the opportunity for bacterial overgrowth, and interfering with enzyme secretion normally provided by the intestine walls.
Damage to the mucous lining of the small intestine increases susceptibility of the gut to macromolecules, promoting the transfer of bacterial toxins from the gut to the portal vein, thus increasing the liver’s exposure to harmful toxins. And last but not least, alcoholism often leads to pancreatitis, a painful condition that causes digestive enzymes to become activated while still in the pancreas, resulting in severe inflammation that can lead to diabetes and complete disruption of the digestive process. (It should be noted, however, that cirrhosis of the liver can also be caused by hepatitis, malnutrition, and other types of infection, which can result in the same liver/gall bladder/enzyme disruption.)
Stress
Although the ultimate effects of stress on the human body are only now being studied in depth, a common complaint among stress suffers involves various types of digestion problems—from constipation to acid reflux, diarrhea to chronic gas. Typically, stress causes the involuntary tightening of stomach muscles, which slows down bowel movement and impedes the digestion process, hindering the body from absorbing essential nutrients. While it is relatively easy to reverse this condition following occasion stressful situations, chronic stress can have far more detrimental consequences.
Frequent stress increases the release of the stress hormone, cortisol. While cortisol is essential in regulating the changes that take place in the body while under stressful circumstances, it also increases belly fat, upsetting the natural chemical balance of the gut. For many, this means increased digestive problems, particularly constipation. When the gut is prevented from emptying, irritable bowel syndrome is also a common result—a condition that further upsets the natural balance of the digestive system, inhibiting the absorption of enzymes and healthy digestive bacteria. Once this pattern is established, digestive enzymes cannot establish or maintain systemic balance.
Medication Overuse/Abuse
In that most doctors suffer a kind of professional tunnel vision when prescribing medication—focused on the primary illness at hand—they seldom consider nor warn patients of the potentially serious consequences of taking prescription or over-the-counter drugs longterm. In reality, continued use of acid blockers (such as Prilosec or Nexium), anti-inflammatories (like aspirin, Advil, and Aleve), and any number of antibiotics, steroids, and hormones beyond one course of treatment, can damage the gut or block normal digestive function, effecting the natural secretion of digestive enzymes. In short, medication overuse/abuse can have a devastating affect on the digestive tract and functioning of digestive enzymes.
Toxicity
Toxins (particularly mercury and mold) can cause serious chemical imbalance to the gut, over-burdening the proper functioning of the liver, gallbladder, and pancreas (including the over-secretion of bile to facilitate digestion), further impairing the digestive process by killing off the good bacteria. Additionally, a growing concern in many parts of the world is the abundance of heavy metals encountered during normal day-to-day interaction with the environment (including their use in vaccination preparation and dental procedures) such as arsenic, cadmium, chromium, and lead–which are known to negatively impact our immune systems, induce multiple organ damage, and are actually classified as human carcinogens. Although certain metals are essential for various biochemical and physiological processes including enzyme formation, our bodies can easily become toxic—creating a serious imbalance of the digestive system.
Magnesium/Zinc Deficiency
Now recognized as much more important to the digestive process than ever considered, magnesium plays a key role in proper functioning of muscles, including those of the lining of the digestive tract. A magnesium deficiency causes the serial smooth muscle contraction of the digestive system (which forces food to move through the digestive tract) to slow down, hindering the movement of bile through the bile duct and urine through the ureters, effectively causing the digestive process to become backed-up (much as a clogged drain). The resulting imbalance confounds the natural enzyme secretion process, blocks the absorption of vitamins, and throws the entire digestive system out of rhythm.
Similarly, when the body suffers a zinc deficiency, the gastrointestinal tract is directly impacted. In addition to contributing to an increased incidence and severity of diarrhea, zinc deficiency creates a susceptibility to toxin-producing bacteria and diminishing absorption of nutrients. Also, zinc deficiency can impair the absorption of water and electrolytes, delaying the course conclusion of normally self-limiting gastrointestinal disease episodes. Again, once this condition manifests, the natural enzymatic balance is thrown off until corrected—and can impact the entire body systemically.
Irritable Bowel Syndrome (IBS)
Reflecting the oft-referenced “chicken-or-the-egg” scenario (which is the cause, which is the effect), the cause(s) of irritable bowel syndrome is not clear, but a variety of factors apparently play a contributing role. While some individuals suffer excessive gas, bloating, and diarrhea—others must endure hard, dry stools, cramps and constipation. Physical abnormalities in the gastrointestinal system may also be a factor—as well as poorly coordinated signals between the brain and the intestines that make individuals overreact to the changes that normally take place during the digestive process. Seemingly triggered by food, stress, hormones, or unrelated disease—science is uncertain whether these factors cause IBS, or IBS is the result of malfunctioning digestive enzymes. In any regard, once this condition manifests it must be addressed in order to return to normal enzymatic functioning.
Heredity and Age Factors
As a result of biological variation, a significant number of Middle-Eastern and Asian-descent individuals lack the enzyme necessary to digest whole milk, which causes bloating, abdominal pain, and osmotic diarrhea. (This enzyme also decreases with aging in Westerners.) Additionally, most individuals experience a general decrease in enzyme production as they age—regardless of ethnicity. In any case, digestive enzymes attempting to compensate for the lack of dairy-tolerant and normal enzyme activity, often throw other enzymes out of rhythm.
Digestive Enzyme Supplements
What Do The Experts Say?
A hot-button topic for many members of the scientific community, a significant number of researchers see the current availability of over-the-counter and mail-order digestive enzyme supplements as nothing more than the supplement industry’s latest ploy to convince consumers to buy supplements they don’t really need. While most gastroenterologists, for example, dismiss over-the-counter digestive enzymes as placebo at best, many health professionals nonetheless recognize a genuine need for prescription enzyme supplements (or enzyme replacements) in specific cases. Brent Bauer, M.D., director of the Mayo Clinic Complementary and Integrative Medicine Program, provides some clarity to the enzyme supplement confusion:
There are clearly medical reasons to use enzymes,”
Dr. Bauer explains.
“If a patient’s pancreas isn’t working, for example, that patient may need to take a medically prescribed enzyme supplement. That’s a little different story from a healthy person who wants to use over-the-counter bromelain or papain–the enzymes that come from the pineapple and the papaya–or trypsin, or chymotrypsin . . . to try to reduce inflammation, maybe help with osteoarthritis.
And there’s a long history of these [enzymes] being used as anti-cancer agents . . . [but] the evidence is pretty limited. We just don’t have the data to say, `No, it doesn’t work. Yes, it does work.’ We’re stuck. If [patients] want to try enzymes, I want them to understand the risks, the potential benefits, the limited amount of evidence. And then if they’re going to use it, I [suggest] a short trial period, use it for two or three weeks. [But even] if you notice a big improvement, it doesn’t mean it works, but it means maybe for you it’s something you might want to continue with. If it’s not working, don’t just keep taking more and hoping for something magical to happen.”
Bauer then warns,
“If you look at some of the bold headlines on dietary supplements–‘Use our enzymes, we can help prevent cancer’–there’s probably a grain of truth . . . but it’s hyped. As soon as you hear that type of hype . . . it’s time to step back and say `Wait a minute, what am I investing my money in?’”
Dr Bauer
Director of Mayo Clniic
Who Should Take Them?
While the need and efficacy of digestive enzyme supplements remains a point of considerable debate, those medical professionals who advocate their use are virtually unanimous as to who should consider using them; which conditions have been shown to improve with their use. Specifically: pancreatic insufficiency, cystic fibrosis, irritable bowel syndrome, and lactose intolerance. Beyond these conditions, the benefits of supplemental digestive enzymes become unclear. And according to the experts, virtually all other treatable conditions are better treated with dietary changes. (Note: Current studies are exploring the possibility of commercially available strains of probiotic bacteria as potentially useful for certain central nervous system disorders.)
Who Type of Enzyme for Which Condition?
Pancreatic Insufficiency (PI), (also, Endocrine Pancreatic Insufficiency (EPI)
This condition, in which the pancreas is unable to produce or excrete normal amounts of digestive enzymes into the intestine, responds well to prescription enzymes taken orally with meals, allowing food to be absorbed. Unlike over-the-counter enzymes, prescription pancreatic enzymes are specially coated to resist being digested by stomach acid before they can accomplish their mission in the intestines. Physicians note that signs of PI include abdominal pain and tenderness, loss of appetite/sensations of fullness, weight loss, (sometimes) diarrhea, and (often) foul smelling, loose stools. Individuals suffering chronic pancreatitis or who have had pancreatic surgery may also benefit from doctor-prescribed supplemental enzymes. (Note: this condition carries a lot of risk factors and should not be self-diagnosed.)
Cystic Fibrosis (CF)
A genetic disorder that primarily affects the lungs but can also affect the intestines, liver, kidneys, and pancreas, cystic fibrosis is known to respond to supplements that contain amylase, lipase, and protease, which help to digest starches, fats, and proteins. Individuals dealing with this condition are generally prescribed enteric-coated pancreatic enzyme capsules (to help prevent being digested by stomach acid before they can accomplish their mission) with dosages ranging from 500 to 4000 units per gram of fat per day. Dosages are often based on body weight, with approximately 2000 units needed per kilogram of body weight for every meal (and half of that for snacks). Thus, doctor diagnosis and prescription is necessary.
Irritable Bowel Syndrome (IBS)
Although the evidence isn’t conclusive, a 1999 study published in Digestive Diseases and Sciences journal found that taking proteolytic enzymes following a high fat meal reduced gas, bloating, and sense of fullness, suggesting possible benefits in using this with irritable bowel syndrome sufferers. However, physicians warn against self-diagnosis and self-prescribing.
Lactose Intolerance
To digest and absorb milk sugar, humans require the lactase enzyme. Biologically, the body decreases its production of lactase soon after childhood, meaning even small quantities of milk and other dairy products cannot be comfortably digested. This (added to the biological reality that digestive enzyme activity gradually decreases with age) supports the general use of a few basic enzyme supplements including over-the-counter and mail-order lactase to compensate for these limitations. It should be noted, however, that many health specialists promote the use of natural substances over supplements to permit dairy consumption (with some questioning the biological need for dairy products after childhood).
When To Take Digestive Enzyme Supplements
According to most sources, unless instructed otherwise by your physician, enzyme supplements should be taken just before eating—without exception.
How To Take Digestive Enzyme Supplements
According to most sources, the recommended/prescribed dosage should always be adhered to. (Do not change the dose without consulting your doctor.) In some cases, slightly higher doses of enzyme supplements may be needed with foods high in fat or when conditions warrant it—which is up to your physician. Report any digestion problems or new symptoms to your doctor immediately.
The Pros, Cons and Side Effects
As explained in the article, “Should You Add Enzyme Supplements to Your Shopping List? Mayo Expert Explains Pros & Cons,” Bromelain, the enzyme derived from pineapple may have anti-platelet activity, meaning individuals taking blood thinners or who have anti-platelet activity may experience an increased risk of bleeding. Also, regarding children suffering cystic fibrosis, a few reported adverse reactions have been reported from patients taking prescription enzymes including manifestation of a colon condition called “fibrosing colonopathy.” And while it may go without saying, a medical doctor should be consulted before taking any digestive enzyme supplement—to avoid wasting money on ineffectual supplements, taking the wrong supplement/wrong dosage, risking bad drug interaction, or taking a supplement that could exacerbate a condition.
Digestive Enzyme Supplements in Perspective
Hype or Helping Hand?
In assessing the overall value or individual need for digestive enzyme supplements, it’s important to keep in mind that categorically, over-the-counter and/or mail-order enzyme supplements garner only minimal support from the medical community at large, and qualified support as doctor-prescribed supplements (specifically in treating lactose intolerance and excessive gas, and in treating pancreatic insufficiency/PI, cystic fibrosis, and irritable bowel syndrome, respectively).
Even in the cases where over-the-counter lactase or pancreatin (a combination of amylase, lipase and protease enzymes) are suggested, long-term use is not a viable option, with most doctors and medical professionals preferring dietary changes to relying on enzymatic supplements. Additionally, there is virtually no professional support for multi-enzyme formulas currently on the market, with only qualified support of commercial probiotics.